Medications for schizophrenia
Medication is an essential component of treating schizophrenia. Medication can help relieve symptoms of schizophrenia such as delusions, hallucinations, and disorganized thinking by blocking certain chemical receptors in the brain.
The most commonly prescribed types of medications for schizophrenia are antipsychotics, and there are two classifications: typical and atypical. These medications sometimes come in various forms, such as tablet, syrup, or injection
What Are Atypical Antipsychotics?
Atypical antipsychotics are also known as second-generation antipsychotics. These medications are generally the first course of medication prescribed because they have a lower risk of serious side effects. They are less likely to cause disorders of movement like tardive dyskinesia, but they may increase the risk of weight gain or high blood sugar (hyperglycemia), which can lead to diabetes.
Atypical antipsychotics include:
Clozaril (clozapine) is a special atypical antispsychotic. Clozaril is usually prescribed only when other antipsychotics fail to relieve symptoms or when a person with schizophrenia suffers from suicidal ideation. This is because there is an increased risk for lowered white blood cell count, and because Clozaril is the only atypical medication that has been shown to help reduce suicidal thoughts. If you take Clozaril, you may need to have your white blood cell count monitored regularly.
What Are Typical Antipsychotics?
Typical antipsychotics were the first generation of antipsychotic drugs to be developed, starting in the 1950s. They can be effective in managing symptoms but also can cause short-term and long-term side effects.
One long-term effect is the development of tardive dyskinesia (TD), which is an involuntary movement disorder. People with tardive dyskinesia may experience random movements in their muscles, eyes, tongue, jaw, and lips. Typical antipsychotics are usually prescribed when atypical antipsychotics have not been effective.
Typical antipsychotics include:
Haldol (haloperidol)
Navane (thiothixene)
Prolixin (fluphenazine)
Thorazine (chlorpromazine)
Trilafon (perphenazine)
Stelazine (trifluoperazine)
Side Effects of Antipsychotics
Side effects of first-generation, or typical, antipsychotics can include:
Sedation
Dry mouth, blurry vision
Dizziness
Weight gain that can lead to metabolic syndrome
Constipation, urinary retention
The most pronounced side effects of these drugs are extrapyramidal, relating to motor activity. Tardive dyskinesia is one of the most distressing ones. The National Alliance on Mental Illness (NAMI) suggests that the risk of developing tardive dyskinesia can be reduced by addressing lifestyle factors like smoking, substance use, and a diet that might lead to high blood glucose levels.
Other extrapyramidal side effects include:
Dyskinesias (uncontrolled, involuntary muscle movements)
Dystonic symptoms (involuntary muscle contractions that cause twisting or repetitive movements)
Akathisia (restlessness)
Akinesia (lack of movement, or rigidity)
Parkinsonism, sometimes referred to as neuroleptic-induced parkinsonism, includes symptoms such as tremor, muscle stiffness, slow gait, problems with posture, and balance and speech difficulties. (This is a different condition than Parkinson’s disease.)
Neuroleptic malignant syndrome is a rare but serious complication of first-generation antipsychotics that causes a variety of side effects that worsen over a period of 24 to 72 hours.
Second-generation antipsychotics are much less likely to cause serious side effects. Because of this, they are generally the first class of drugs that are prescribed to someone experiencing a psychotic illness.
However, they are associated with increased weight gain as well as an increase in triglycerides (blood fats) and other metabolic side effects.
They can also increase the risk of diabetes. They can cause some people to have activating side effects (feeling jittery) or sedating ones such as sleepiness, slowness of thought, and difficulty concentrating.
Symptoms of Schizophrenia
When prescribing medication, doctors aim to provide the drug that eases the most symptoms of a condition, with the fewest side effects, and in the most tolerable dose. Symptoms of schizophrenia that can be addressed with medication include “positive” and “negative” symptoms.
Positive Symptoms
These add a feeling or behavior that isn’t typically experienced by most people without schizophrenia, such as delusions or hallucinations.
The experience of positive symptoms in schizophrenia designates a break with reality and is referred to as psychosis. Patients can experience either hallucinations or delusions, or both simultaneously.
Hallucinations are the experience of visual, auditory, or olfactory sensations that others cannot see, hear, or smell. Auditory hallucinations can include hearing a voice or voices in one’s head, which the person does not identify as their own internal voice or thoughts. These voices can be disparaging and threatening.
Delusions are firmly held irrational beliefs that the patient upholds despite evidence to the contrary. Common forms of delusions in schizophrenia include:
Delusions of persecution. This is a strongly held belief that someone or something means to do you physical or emotional harm. An example of a delusion of persecution is believing that your next-door neighbor is entering your home while you are sleeping in order to poison your food or to spy on you.
Delusions of grandeur. This is a belief that you are an important, powerful, or famous person. That could mean that you are royalty, a historical figure, or even a deity. You may believe you also have special powers, such as an ability to know the future.
Delusions of reference. You feel that something or someone is referring to you when it is not. These delusions can take on many forms. For instance, you may believe something you read in the newspaper refers to you or your thoughts. An actor talking in a movie may seem like they’re sending a message to you personally. Neutral or innocuous stimuli seem to take on personal and possibly harmful significance.
Thought insertion. This is the belief that your thoughts are not your own, rather they were placed there by an outside source. This is similar to auditory hallucinations; someone with schizophrenia can attribute internal stimuli—like their thoughts—as coming from an external source.
Thought broadcasting. One may feel as though their thoughts are not being privately contained inside their own mind. Instead their thoughts are being broadcast so that someone or something can observe or collect them. This could be literal broadcasting, such as the belief that aliens are projecting your thoughts into outer space via radio waves. It could also mean a general feeling that people around you know your thoughts without you having to speak or share them.
A psychotic person is not aware of the bizarre nature of his or her delusions or hallucinations. They cannot simply be “talked out” of these beliefs, or be made to shown how they are untrue. That’s because their mental condition causes what’s called anosognosia, which means a “lack of insight” into a mental health condition. It may seem plainly untrue to someone not suffering from schizophrenia that the mail carrier would be sending hidden messages to you via weekly circulars, but a person with schizophrenia cannot see why this is illogical.
Someone with schizophrenia may also experience disorganized speech, such as incoherence, perseveration (the repetition of words), frequent derailment (touching on unrelated or loosely associated ideas), or word salad (an unintelligible mixture of nonsense or made-up words). They may display grossly disorganized or catatonic behavior, including stupor or extreme rigidity or flexibility of the limbs.
A negative symptom takes away a feeling or ability that is normally present in most people, but is now missing—such as a lack of motivation. Negative symptoms of schizophrenia include:
Avolition. Lack of motivation, inability to follow goal-oriented action.
Anhedonia. Inability to experience pleasure.
Social withdrawal. No interest in being with other people.
Difficulty paying attention.
Apathy. This can show up as lack of personal hygiene or a lack of concern for others or self.
Affective flattening. An absence of emotional expression facially, vocally, even a lack of body language.
Alogia. Reduction in speech, little detail used when communicating.
Someone suffering from schizophrenia could experience any combination of positive or negative symptoms. Symptoms tend to persist or occur separately from those of a mood episode like severe depression or bipolar mania.
People with schizophrenia also often experience impaired executive function, including working memory. This means they may be unable to process, interpret, and retain new information or recall this information in order to perform a task later. Deficits in attention and short-term memory are common.
Antidepressants for Schizophrenia
People with schizophrenia are also sometimes prescribed antidepressants to manage low-mood symptoms or negative symptoms.
A 2019 study published in JAMA Psychiatry found that people with schizophrenia who were given an antidepressant in addition to an antipsychotic medication were 16% less likely to be hospitalized for a mental health issue than those on antipsychotics alone, and 22% less likely than people taking an antipsychotic and benzodiazepine.
Antidepressants that may be prescribed in schizophrenia include:
Selective serotonin reuptake inhibitors (SSRIs) fluoxetine (Prozac), fluvoxamine, and citalopram (Celexa)
Serotonin antagonist and reuptake inhibitor (SARI) trazodone (Desyrel)
Serotonin 5-HT2C antagonist ritanserin
Tricycyclic antidepressant (TCA) amitriptyline (Elavil)
Atypical antidepressant bupropion (Wellbutrin)
Mood Stabilizers in Schizophrenia
Mood stabilizers may also be prescribed. These are typically used to treat bipolar disorder but have shown some effectiveness in addressing psychotic symptoms of schizophrenia, such as hallucinations, delusions, and disordered thinking.
Common mood stabilizers are carbamazepine (Tegretol), valproic acid (Depakote), lamotrigine (Lamictal), and lithium.
What to Know About Medication Management
It’s important to talk to your doctor about any other medications you are taking or medical conditions you have before taking antipsychotics. All antipsychotics have the potential to cause cardiac complications, so be sure to talk to your doctor about the risks and get regular checkups.
Doctors also recommend that you not discontinue use of antipsychotics before consulting with them. Let your doctor know if you’re experiencing any side effects. You can also report side effects to the FDA at 1-800-FDA-1088 or online.
Try to not be discouraged if the first antipsychotic prescribed is not as effective in managing symptoms. Often it takes several tries before patients find the best medication that works for managing their form of schizophrenia.
Antipsychotic medications can reduce or relieve symptoms of psychosis, such as delusions (false beliefs) and hallucinations (seeing or hearing something that is not there). Formerly known as major tranquilizers and neuroleptics, antipsychotic medications are the main class of drugs used to treat people with schizophrenia. They are also used to treat people with psychosis that occurs in bipolar disorder, depression and Alzheimer’s disease. Other uses of antipsychotics include stabilizing moods in bipolar disorder, reducing anxiety in anxiety disorders and reducing tics in Tourette syndrome.
Antipsychotic medications can help to calm and clear confusion in a person with acute psychosis within hours or days, but they can take up to four or six weeks to reach their full effect. These medications can help to control symptoms, but they do not cure the underlying condition. When taken over a longer term, antipsychotics can help to prevent further episodes of psychosis.
While antipsychotic medications can help some people with psychosis and mood disorders, these drugs can have serious side-effects. The aim of medication treatment is to reduce and control symptoms while keeping side-effects at a minimum.
Combining antipsychotic medication with other therapy and support can help people to manage symptoms and improve quality of life. Family therapy, peer support, school and job counselling, and housing and employment supports can all be helpful. Some therapists now offer cognitive-behavioural therapy to help people cope with voices and other auditory hallucinations.
Taking care of your physical health is especially important if you take antipsychotic medication. Both schizophrenia and the medications used to treat it can increase the risk of diabetes and other serious health problems. Getting regular checkups and medical care can help you to have good physical health. Eating a nutritious diet, exercising regularly and getting enough sleep can also help you to get and stay well.
Do I need this treatment?
Psychosis; can be dangerous, frightening, isolating and disabling. Symptoms of psychosis, such as delusions and hallucinations, may come on gradually and build up over time, or they may come on rapidly. People experiencing psychosis may not be aware that the experiences they are having are not normal. To them, what is happening in their minds is very real.
Recognizing and treating psychosis in the early stages greatly improves a person’s ability to recover and to lead a satisfying and rewarding life. Family, friends, colleagues and health providers play an important role in recognizing the signs of psychosis and in encouraging the person to get treatment. However, the symptoms of psychosis can sometimes lead to a breakdown in the person’s relationships with the people who might be most able to help him or her get treatment. Family members and others who support a person with psychosis may wish to seek support themselves, for example, from a family support group.
People with anxiety and mood disorders may benefit from taking antipsychotics in addition to antidepressants or mood stabilizers. When used in this way, antipsychotics may help to control symptoms such as irritable or depressed mood, disorganized thinking, and trouble concentrating and remembering.
What does Antipsychotic Medications do?
Psychosis is believed to be caused, at least in part, by overactivity of a brain chemical called dopamine, and antipsychotics are thought to work by blocking this dopamine effect. This blocking helps to make the symptoms of psychosis—such as voices and delusions—less commanding and preoccupying, but it does not always make them go away completely. People may still hear voices and have delusions, but they are more able to recognize what isn’t real and to focus on other things, such as work, school or family.
Side effects of Antipsychotic Medications
Antipsychotic medication can cause unpleasant side-effects, especially when the symptoms are severe and a higher dose of medication is used. Side-effects should become mild or at least tolerable when the dose is reduced and as your body adjusts to the presence of the drug.
Most side-effects will go away when you stop taking the drug. There is a risk, however, of a condition that causes people to make involuntary movements, known as tardive dyskinesia, which can be permanent.
Some people accept the side-effects as a trade-off for the relief these drugs can bring. Others find the side-effects distressing and may choose not to take the medication.
Check the information given to you by your doctor or pharmacist to find out the specific side-effects of any drug you have been prescribed. If you are troubled by any of these effects, it is best to continue to take your medication as prescribed and let your doctor know as soon as possible. Your doctor may:
- adjust your dose
- prescribe other medications to help control side-effects
- change your medication.
Side-effects of antipsychotics
- Movement effects: Tremors, muscle stiffness and tics can occur. The higher the dose, the more severe these effects. The risk of these effects may be lower with the second generation medications than with the older drugs. Other drugs (e.g., benztropine [Cogentin]) can be used to control the movement effects.
- Dizziness: Feelings of dizziness may occur, especially when getting up from a sitting or lying position.
- Weight gain: Some of the second generation drugs are thought to affect people’s sense of having had enough to eat. They can also be sedating. These two effects can result in weight gain, which can increase a person’s risk of diabetes and heart disease.
- Diabetes: Schizophrenia is a risk factor for diabetes. Antipsychotic drugs can increase this risk.
- Agitation and sedation: Some people feel “wired” and unable to stop moving when taking antipsychotics. This effect may be mistaken for a worsening of illness rather than a side-effect of the medication. These same drugs can also have the opposite effect, making people feel tired. Some people may feel either wired or tired, and some may feel both at the same time.
- Tardive dyskinesia: For every year that a person takes antipsychotic medication, there is a five per cent chance of developing tardive dyskinesia (TD), a condition that causes people to have repetitive involuntary movements. The risk of TD is highest with the first generation antipsychotics, although it can occur with the second generation drugs. TD can worsen when you stop taking medication and can be permanent .
- Neuroleptic malignant syndrome: This rare but serious complication is usually associated with the use of high doses of typical antipsychotics early in treatment. Signs include fever, muscle stiffness and delirium.
Side-effects vary depending on the type of medication. More information on side-effects is included with each type of antipsychotic.
Controlling the side-effects of antipsychotics
You can help to control possible side-effects on your own by:
- getting regular exercise and eating a low-fat, low-sugar, high-fibre diet (e.g., bran, fruits and vegetables) to reduce the risk of diabetes and help prevent weight gain and constipation
- using sugarless candy or gum, drinking water, and brushing your teeth regularly to increase salivation and ease dry mouth
- getting up slowly from a sitting or lying position to help prevent dizziness.
Types of Antipsychotic Medications
NOTE: medications are referred to in two ways: by their generic name and by their brand or trade names. Brand names available in Canada appear in brackets.
Antipsychotic medications are generally divided into two categories:
- atypical (second generation) antipsychotics
- typical (first generation) antipsychotics
The main difference between the two types of antipsychotics is that the first generation drugs block dopamine and the second generation drugs block dopamine and also affect serotonin levels. Evidence suggests that some of the second generation drugs have milder movement-related side-effects than the first generation drugs.
Both categories of drugs work equally well overall, although no drug or type of drug works equally well for everyone who takes it. When the same drug is given to a group of people, one-third of that group will find that it works well; another third will find that the drug helps only with some symptoms; and the final third will find that it does not help at all. For this reason, people may need to try different antipsychotics before finding the one that works best for them.
Most of these drugs are given in tablet form, some are liquids and others are given as injections. Some are available as long-lasting (depot) injections, which may be given anywhere from once a week to once a month.
Most people who take antipsychotics over a longer term are now prescribed the second generation (also called atypical) drugs.
Atypical antipsychotics
The second generation antipsychotics are usually the first choice for the treatment of schizophrenia. Although they may not be officially approved for these other uses, they are sometimes used in the treatment of mood and anxiety disorders, such as bipolar, posttraumatic stress and obsessive-compulsive disorders.
Medications available in this class include risperidone (Risperdal), quetiapine (Seroquel), olanzapine (Zyprexa), ziprasidone (Zeldox), paliperidone (Invega), aripiprazole (Abilify) and clozapine (Clozaril).
Clozapine is exceptional in that it often works even when other medications have failed; however, because it requires monitoring of white blood cell counts, it is not the first choice for treatment.
Possible side-effects of atypical antipsychotics include:
- Dry mouth
- dizziness
- blurred vision
- seizures (rarely)
The following list details other side-effects of atypical antipsychotics and which drugs are most likely to least likely to have these effects.
Weight gain, diabetes: clozapine > olanzapine > quetiapine > risperidone > ziprasidone, aripiprazole
Movement effects (e.g., tremor, stiffness, agitation): risperidone > olanzapine, quetiapine, ziprasidone, aripiprazole > clozapine
Sedation (e.g., sleepiness, low energy): clozapine, olanzapine and quetiapine > risperidone, ziprasidone, aripiprazole
Decreased sex drive and function, missed periods, discharge from breast: risperidone > olanzapine, quetiapine > clozapine, ziprasidone
Typical (first generation) antipsychotics
These older medications include chlorpromazine (once marketed as Largactil), flupenthixol (Fluanxol), afluphenazine (Modecate), haloperidol (Haldol), loxapine (Loxapac), perphenazine (Trilafon), pimozide (Orap), trifluoperazine (Stelazine), thiothixene (Navane) and zuclopenthixol (Clopixol).
Side-effects of typical antipsychotics vary depending on the drug and may include drowsiness, agitation, dry mouth, constipation, blurred vision, emotional blunting, dizziness, stuffy nose, weight gain, breast tenderness, liquid discharge from breasts, missed periods, muscle stiffness or spasms.
Frequently Asked Questions
How long should I take antipsychotics? If you take antipsychotics for psychosis, how long you take them depends on what the psychosis is related to and how many episodes you have experienced. In some situations, you may only need to take this medication until the symptoms of psychosis are relieved. In others, antipsychotics may be used over a longer term to help prevent further episodes. Drugs that are addictive produce a feeling of euphoria, a strong desire to continue using the drug, and a need to increase the amount used to achieve the same effect. Antipsychotics do not have these effects. How do I cut down or stop taking antipsychotics? Whether you want to cut down your dose or stop taking a medication, the same rule applies: go slowly. A sudden change in your dose greatly increases the risk that psychotic symptoms will return or become more intense. Will antipsychotics interact with other medications? What if I smoke cigarettes or drink coffee or alcohol while taking antipsychotics? What if I use street drugs while taking antipsychotics? |
Treatment Guidelines
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
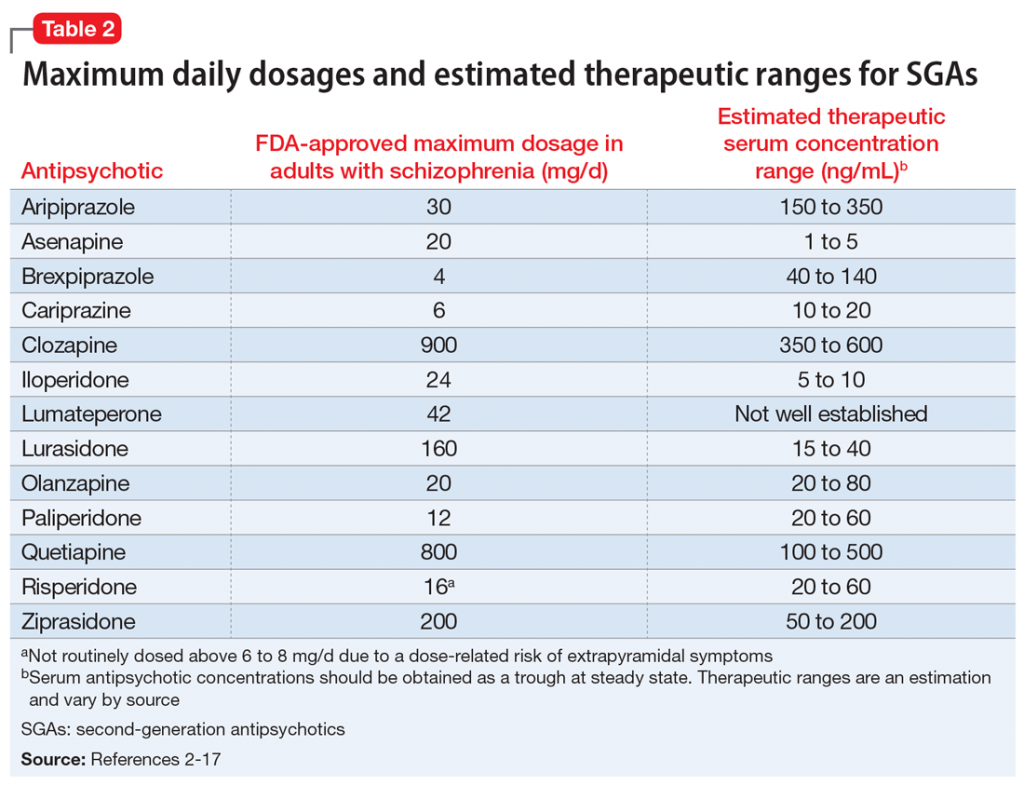
Therapeutic Drug Monitoring
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
Powered By EmbedPress
